Hypochlorhydria (low stomach acid)
Many people understandably believe that the acidic burning sensation symptomatic of heartburn is a result of too much stomach acid, because it seems intuitively true, and because the pharmaceutical industry spends billions trying to persuade you that this is the case.
However, the opposite is true.
Too little stomach acid, also known as hypochlorhydria, is the source of many downstream digestion and absorption issues, including heartburn and reflux.
The symptoms of heartburn are caused by stomach acid, and these symptoms are temporarily alleviated by acid suppressing drugs, either H2-receptor blockers: Cimetidine (Tagamet), Ranitidine (Zantac) etc. or proton pump inhibitors: Omeprazole (Prilosec), Lansoprazole (Prevacid), but these drugs do not address the root cause of the problem.
Here’s why.
You need stomach acid to adequately break down the food you eat. If you’ve just had a steak, or chicken breast, that protein needs to be chemically digested, and stomach acid, otherwise known as hydrochloric acid (HCl) is going to stimulate the release of pepsin in order to begin the process of breaking down protein and releasing all the vital minerals and vitamins that come with it. You need stomach acid to absorb iron, zinc, copper, calcium, B12, and folic acid. You need stomach acid to send downstream signals to other parts of your digestive system to release enzymes to further break down protein, carbohydrates and stimulate the release of bile to emulsify and absorb fats.
The importance of proper digestion cannot be overstated. It begins in the mouth, of course, with proper chewing, but the stomach is next in line, and if it cannot do its job properly, the downstream consequences can range from constipation, gas, bloating, indigestion, to more serious concerns, such as autoimmune conditions. If protein fragments are not properly broken down, you are not releasing the building blocks of protein, which are amino acids and peptides.
These larger than usual fragments of partially digested proteins can also squeeze their way through the one-cell thick lining of the colon and into the bloodstream, where your immune defence is waiting to attack. These fragments are often considered as foreign invaders by the immune system and tagged for destruction. The problem is, organ systems and tissues are comprised of protein, and sometimes these proteins are very similar to the undigested protein fragments leaking through your gut. The thyroid gland, for instance, can be confused with the protein gliadin, or gluten, so the immune reaction will start to tag the thyroid gland for destruction. I’m skating a little bit outside the rink here, so let’s move back to the subject at hand: low stomach acid, otherwise known as hypochlorhydria.
The bottom line is having a stomach full of stomach acid is good news.
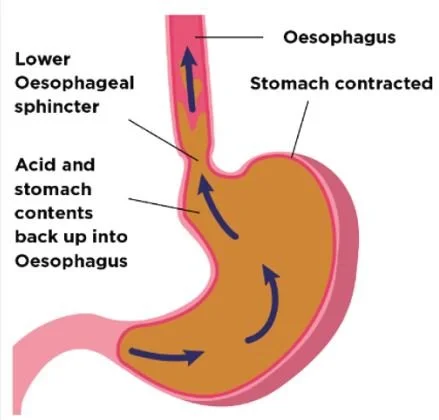
But having a weak LOS is not. Once you’ve chewed your food, it travels down the oesophagus and enters the stomach through the lower oesophageal sphincter (LOS).
There are certain things (aside from eating and burping) that make the LOS open up and allow stomach acid to intrude into the oesophagus. This is not because you have too much stomach acid. If you have ANY stomach acid, this would happen.
One of these things is intra-abdominal pressure (IAP). In the diagram, you can see the stomach is contracted, but just before the contraction, the stomach can inflate like a balloon, creating an uncomfortable bloating sensation. IAP can happen as a result of having eaten too much, obesity, or because you’re slunk on the sofa in a post-meal coma.
If you’ve been taking acid suppressing drugs over the course of many years and if you’ve also been aging, which I suspect you have, then you can reliably expect to have a sub-optimal level of stomach acid, and therefore problems digesting the food you’re eating. Other factors that can cause low stomach acid are chronic stress, and H. pylori infection, which is incredibly common, and which I’ll talk about in a separate article.
You might be aware that fiber is a non-digestible carbohydrate and is therefore fed upon by gut microbes. Well, any carbohydrates that are not broken down and absorbed as a consequence of decreased stomach acid, (or increased stomach pH) will also be fermented by gut microbes. Most of your gut microbes are located in the colon, but if these opportunistic little fellas detect undigested carbohydrates in the small intestines, they will start migrating north.
In this case, the gut microbes, or bacteria, will start to thrive in the small intestine, because they’re well fed with undigested carbohydrates. This leads to a condition known as small intestinal bacterial overgrowth (SIBO).
Here’s how all this relates to heartburn and acid reflux. When bacteria ferment carbohydrates, they produce gas, and this gas causes intra-abdominal pressure which causes stomach bloating. When the stomach subsequently contracts, it pushes stomach acid up through the LOS and causes heartburn.
It should become clear now that taking acid suppressing drugs will only make the problem worse because the root cause is improperly digested food as a result of either inadequate levels of stomach acid or the environment of the stomach is not acidic enough.
Here are some possible symptoms of low stomach acid:
Bloating, belching, burning and flatulence immediately after meals
Dilated blood vessels in the nose and cheeks (Rosacea)
Excess gas in the upper intestine
Indigestion, diarrhoea or constipation
Iron deficiency
Multiple food allergies
Nausea after taking supplements
Peeling or cracking fingernails
Rectal itching
Sense of “fullness” after eating
Undigested food in the stool
If you are frequently experiencing some of these symptoms, it might be helpful to start taking HCl supplements. Here is some advice on how to go about supplementing with HCl:
Find supplements with at least 600 mg of betaine HCl per tablet or capsule
Start with one right at the beginning of a meal or immediately after beginning to eat.
At every meal after that, use one more pill
Continue until 5 tablets/capsules are consumed with each meal, or until warmth occurs in the stomach, whichever happens first.
The warm feeling indicates too many were consumed, so cut back by one pill at the next meal.
Smaller meals need fewer pills, larger meals, more
If you need 5 or so capsules you should spread them throughout the meal
After while, and after repairing the digestive system, you may start producing your own HCl and so need fewer capsules.
So, I hope this information helps! If you have any questions, hit me up in the comment box below.